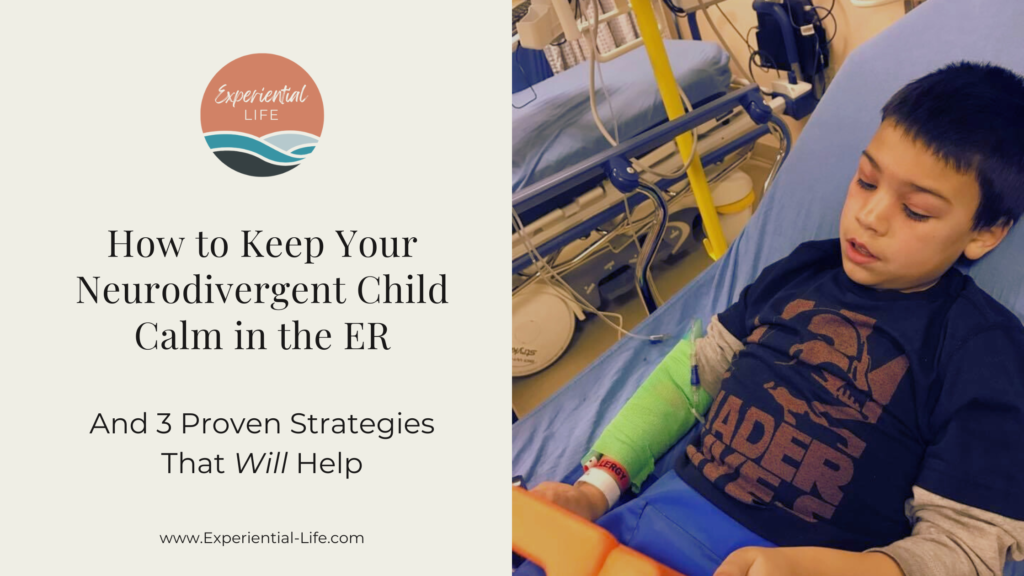
How to Keep Your Neurodivergent Child Calm in the ER
- by Christy
How to Keep Your Neurodivergent Child Calm in the ER
“Should we go to the ER?” I asked, as I watched his face get redder and more swollen.
C, my neurodivergent son, woke up rubbing his eyes. It seemed normal at first. Who doesn’t give their eyes a good rub to shake the dreams away and confront the day?
But then he wouldn’t stop rubbing his eyes, then his cheeks, then his neck.
Red, angry blotches started to cover the upper half of his body. His eyes started to swell, and clearly, he needed medical attention.
The Warning Signs
We believe C doesn’t feel pain in the same way we do. He won’t complain of sickness until a fever takes hold. He can get cuts and bruises that would put tears in most grown men’s eyes, and he barely notices – until blood starts to drip.
Or maybe it’s hard for him to communicate that he doesn’t feel good. He has a hard time finding words to describe the source of pain, what the pain feels like, and how long he hasn’t felt well.
This day was no different. He seemed more tired than usual, but did not complain. He just kept rubbing and scratching and was restless despite his need for snuggles.
We tried cold compresses, Benadryl, and a bath. Of course it was the weekend, right before the holidays, so the pediatrician’s office was closed.
Then he started coughing.
I called a nurse friend for help.
“What should I do?”
“It sounds like an allergic reaction, and if he’s coughing, he might be going into anaphylaxis. Take him to the ER,” she said.
Before Heading to the Hospital
This was the year of hospital visits. My oldest showed signs of pneumothorax (hole in the lung) after a wrestling tournament. An ER doctor diagnosed my middle son’s stomachache as intussusception (when the intestine turns inward on itself), but before the helicopter came to pick him up, a second surgical consult cleared him of the condition.
At this point, the pediatric nurses in the ER knew us, and we knew them.
I narrated to C as I packed up the essentials. I wanted him to know where we were going and why. I quickly put together a backpack with:
➤ Water bottles
➤ Phone chargers
➤ iPad
➤ Snacks
➤ Comfy blanket
➤ Mickey plush that attends all the doctors visits
My husband stayed with the older boys and C and I jumped in the car to head to the hospital.
3 Proven Strategies to Keep Your Child Calm in the ER
When we got to the hospital, we rushed right to the Pediatric ER.
The first thing I did was let the nurses know about C’s diagnosis and provided a bit of background on the escalation of his symptoms, his communication style, and how his autistic traits interact with stress. This is a very personal decision. Some families feel more comfortable NOT disclosing the diagnosis – but in this situation, disclosing C’s diagnosis felt important.
Because of his symptoms, he went right to triage and then to a room. Shortly after, three more nurses and another woman, who introduced herself as a social worker appeared, and friends… what they did next changed everything!
Strategy 1: Child Life Specialist
A Child Life Specialist is a health care professional who is trained in the emotional and developmental needs of children. They help children and their families understand medical issues and give psychological and emotional support.
And did we need emotional support – because behind the child life specialist was a nurse with a bag of saline and an IV needle.
The child life specialist introduced herself to C and explained why she and three other nurses were in the room. She then explained that they needed to help his body feel better and one of the ways to do that was through a needle in his arm that could deliver medicine.
Strategy 2: Explain What to Expect, What is Happening, and Why – to Your Child
Better communication between medical providers and patients leads to better health outcomes. There is a ton of research that supports this – and it is also true for neurodivergent pediatric patients.
The fact that the child life specialist came in and talked to C first, was a first for me. Most medical providers talk to me first and speak as if my son isn’t even in the room. I can’t know for sure, but I imagine that my son’s anxiety increases when people talk about him, not to him, when he is sitting right next to them.
As the nurses prepared the IV, the child life specialist continued to talk to C, and only asked me for clarification about what he said.
Strategy 3: Sensory Items
A recent study from the School of Medicine, University of Alabama at Birmingham, showed improved patient experience by “having [sensory] tools readily available to aid with sensory regulation and comfort of patients during healthcare encounters.”
So when one nurse approached C with a needle in her hand, my heart rate increased… until the next nurse came over with a toy bee that buzzed. And the third nurse approached with an iPad and lidocaine spray.
The child life specialist introduced her three nurse “friends” and explained again that they would need to help C by putting medicine right into his body. The nurse with the buzzing bee let C hold it, buzz it on his arm, and put it on my arm so I could feel it too. Then the nurse with the lidocaine spray and iPad approached. She showed C the can and explained that it would make the area where they wanted to put the shot not feel pain. She offered the iPad, but he was happy with his own.
And ya’ll… He let her spray his arm. He let the buzzing bee flitter along the area that they wanted to put the IV, and then the two nurses talked and talked about the game C was playing on his iPad, while the nurse with the IV successfully inserted the needle. She had his arm wrapped and the saline bag dripping before he even knew something happened!
I know, I know – this isn’t always the case. I expected him to rip the IV right out from beneath the green gauze that held it in place. The tears, quick escape, and chase down the hospital hallway I expected, never happened.
Maybe it was because they explained to him exactly what to expect, when, and why 🤷♀️
All I know is that whatever the doctor said, I felt like we were in good hands.
Managing the Emotions of a Really Scary Diagnosis
When the doctor came in with a grim look on her face, I felt all the relief turn into panic.
She said that they thought C had Stevens-Johnson Syndrome, a skin disorder that causes flu-like symptoms, a rash that blisters, and eventually leads to the skin peeling away.
Google was not my friend. I immediately understood the grim look on the doctor’s face.
They needed to run more tests, which meant a blood draw.
And I needed to wait for the results.
Those moments will forever remain etched in my brain.
Again, it was the year for really scary diagnoses that turned out to be not so scary at all – but the resulting trauma of thinking your child is in a life-threatening situation doesn’t go away.
This was no different, and I feared our luck was running out.
I called my nurse friend back and asked for her thoughts. “I bet it’s out of an abundance of caution. Stop Googling!” she said.
As it turned out, she was right. The tests did not show the super scary Stevens-Johnson Syndrome. Instead, they diagnosed him with an allergic reaction, gave him antihistamine through his IV, and sent us home.
Improve Communication with Your Child's Medical Team
Maybe the medical team’s intentions were good. Provide timely updates based on what we see right now… Prepare mom for the potentially life-threatening prognosis…
But the delivery and after shocks of those conversations sucked.
How that conversation played out affects how I communicate with medical professionals now.
I am always braced for the worst possible outcome, and fearful that I am over reacting.
Because after tests confirmed my child’s life was not at stake, the docs sent me home with instructions to monitor his condition and come back if it gets worse.
So, I didn’t sleep.
I still check on him, years later, when he sleeps in – as teenagers do – to make sure he is still breathing.
This is why I am hosting a conversation with Tiffany Ryder, PA-C. As a former Emergency Room Physician Associate, she’ll pull back the curtain talk to us about her experience working in the emergency room, and how we can improve communication with our child’s medical team.
You’ll walk away from the conversation with a better understanding about how medical providers process what you tell them and how that guides their clinical decisions.
It’s sure to be both informative and entertaining. Tiffany is a brilliant storyteller and ties anecdotes from her time in the emergency department to actionable steps we can take to better advocate for our kids.
Experiential Life community members can find the conversation in the resource library, or join the conversation live on August 27, 2024 at noon EST.
If you aren’t a member with access to the app – join the waitlist today!